I’ve partnered with the American Gastroenterological Association (AGA)’s IBD Parenthood Project to bring you this blog post.
If I’ve learned anything from motherhood, it’s that in order to raise a healthy baby, I needed to be a healthy mom first. My experience with pregnancy and inflammatory bowel disease (IBD) was relatively lucky, but everyone’s journey is different. IBD Parenthood Project aims to address misperceptions and fears women with IBD and their health care providers experience throughout all phases of family planning (conception, pregnancy and after delivery). The projectbrings together all women regardless of how easy or difficult their journey is, and the resources are invaluable. Knowledge is power and the more informed we are, the more confident we can be with the decisions we make for ourselves and our children.
If you’re struggling with IBD, thinking about starting a family and don’t know where to start, I recommend visiting www.IBDParenthoodProject.org for their valuable resources. The resources have been wonderful for both me and my friend Abby, teaching us a thing or two! Abby Bales is a fellow ulcerative colitis patient, mom of two, Doctor of Physical Therapy, Certified Strength and Conditioning Specialist, runner, coach, wife, and mid-western gal living in New York City. She writes the blog Run Stronger Everyday, and she was one of the first (maybe the first) person I connected with after my ulcerative colitis diagnosis. Abby is an IBD advocate and extremely involved within the IBD community. She was – and continues to be – one of my go-to sources of support when it comes to navigating my disease. I am so thankful that she agreed to share her story here on Carrots ‘N’ Cake. I hope you’ll learn something new from Abby’s experience. Please pass this story onto anyone you know who might benefit from IBD Parenthood Project resources.
Abby’s Story
I was saddened to learn that the percentage of women with IBD who are voluntarily childless is three times greater than the rest of the general population, and I can totally relate because I was hesitant to start a family as well. With a resource like IBD Parenthood Project, women with IBD can rest easy knowing that they have a supportive place to turn to when they have questions, concerns, or just want more information.
Hi there! My name is Abby Bales and I have ulcerative colitis. I mean, I have no colon NOW, but I still technically have the disease and carry all the risks with me to this day, 7 years after my colectomy. I’m also a mom of a 2-year-old and 5-year-old, a business owner, and a wife.
My story with IBD starts a little over 9 years ago, 6 months after my husband and I were married, 2 months before I was to go back to school for my pre-med, and 1 month before my 30th birthday. I saw blood in my stool and due to a family history of colon cancer, I demanded a colonoscopy from my gastroenterologist (GI), which ended up with a diagnosis of “mild colitis” that sent me running to an IBD specialist. I live in New York so there are plenty of specialty doctors available in the area; however, not everyone will have close access to IBD experts. But don’t worry IBD Parenthood Project developed a clinical care pathway that you can print and give to your doctor to read and help guide your care during family planning. There is also a link on their site to help you find specialists in your area!
Lots of people newly diagnosed with IBD have tons of questions, I know I did. Among many of the questions I had for my doctor surrounding my diagnosis, testing, and proposed treatment was, “Would I be able to have kids?” I remember him so clearly saying, “We have a very fertile practice here…” He pointed to a wall that was full of pictures of the children of patients at the practice.
He told me about how the immune system can sometimes settle down during pregnancy and bring on remission or flare up and get worse with a growing baby. But he assured me that my specific medications would be safe to use during pregnancy and we would tackle any uncertainties that might arise while my husband and I grew our family. As is the same for most IBD patients, I went through step therapy of treatments and drugs over the course of the next 2 years. Unfortunately, I was resistant to all medications. As a result, I was guided by my GI team to have a colectomy and a J-pouch surgery.
I felt defeated. I remember sobbing in the office with Dr. Bosworth’s PA letting me unload my fears onto her. Would I have to have a colostomy bag forever? If I did, would I be able to have children? Isn’t there a risk of infertility with an abdominal surgery so close to my uterus and fallopian tubes? Did I have to have a c-section with a J-pouch? Am I high risk pregnancy now? Will my babies be healthy? Will they have IBD too?
She told me in no uncertain terms that women with IBD, J-pouches, K-pouches, and permanent and temporary colostomy bags have successful, healthy pregnancies every single day. But I needed surgery if I was ever to be healthy enough to carry a pregnancy to term.
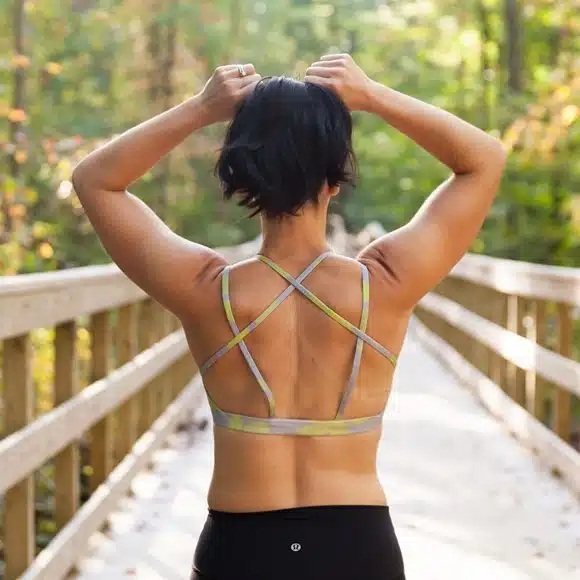
So, off I went and had the colectomy, recovered, started my program, had my ileo-anal anastomoses (J-pouch take-down), ran a half-marathon PR 7 months later, and was pregnant without any medical intervention 3 months after that. I felt like I had put my IBD behind me.
At 34 weeks pregnant with our son, I had a bowel obstruction and was hospitalized. They couldn’t explain the obstruction, decided to treat it conservatively and wait, and it eventually resolved itself. Crisis averted.
When discussing delivery options with my MFM Ob and Dr. Bosworth, we all agreed that, while I could attempt a vaginal delivery, I didn’t think I should. I am a pelvic health physical therapist, so my training and education pointed me toward a c-section right away. Also, I come from a family of people with large heads and wasn’t super excited by the prospect of having a giant baby potentially tear my rectum and compromise my J-pouch. Were that to happened, I’d be whisked off the OR to repair the pouch and have my postpartum recovery further derailed by my own health. I wasn’t willing to take this chance and elected for the c-section.
On June 3, 2014, I was safely delivered of a son via c-section. Two years later, I was pregnant with our second baby and in a much more precarious position. Dr. Bosworth had moved his practice to NYU-Tisch Hospital as the Chief of Medicine, where I followed him like some crazy stalker, and thank goodness I did. Because at 16 weeks gestation with our daughter, I had another bowel obstruction.
Despite a complicated pregnancy involving multiple bowel obstructions and GI surgeon oversight, I was able to carry my daughter full term, deliver her via c-section, and then get down to the business of finding out why I kept getting sick, even after the babies were delivered.
After additional surgeries to resolve the cause of my constant bowel obstructions, I’m better than I was before. Better than I thought I could ever be. I’m back to running, to chasing my crazy monsters, to running my practice, to life.
People ask me all the time if I was scared to have surgery. At first, I really was. Everything about my disease felt unknown to me at every turn. I went from diagnosis to surgery in 2 years and felt isolated and alone much of that time. I didn’t know about and wasn’t able to fully take advantage of the support available then and the multitudes of support systems that have been created since through Girls With Guts, the Crohn’s & Colitis Foundation (CCF), or the AGA IBD Parenthood Project. I feel like even my MFMs weren’t super familiar with my disease and surgeries back when I was pregnant. Now, I feel like every person I meet knows someone with IBD. I mean, there ARE 1.6 million of us and half of those are female, so it stands to reason everyone will know someone with IBD.
I want my story to be told and my voice to be heard. I want women to start the conversations with their obstetric providers and GIs and surgical team about fertility, pregnancy, and postpartum recovery sooner rather than later. I want women to know children won’t automatically get IBD from mom or dad, but it’s a combination of genetics and environment, not gestation or delivery method, that cause someone to develop the disease.
Most of all, I want all of us to continue to fight the stigma of the disease and keep lending our voices and efforts to finding more effective treatments and a cure. While we’re doing that, though, let’s also have babies.